In spite of that, in today’s inactive world where almost every indispensable job can be carried out on-line, from the ergonomic chair in front of a computer, or with a streaming line of messages from a fax machine, exercising can be a hard argument to win over.
The Weight of Exercise
Everyone should exercise, yet the health experts tells us that only 30% of the United States population gets the recommended thirty minutes of daily physical activity, and 25% are not active at all. In fact, inactivity is thought to be one of the key reasons for the surge of type 2 diabetes in the U.S., because inactivity and obesity promote insulin resistance.
The good news is that it is never too late to get moving, and exercise is one of the easiest ways to start controlling your diabetes. For people with type 2 diabetes in particular, exercise can improve insulin sensitivity, lower the risk of heart disease, and promote weight loss.
Type 2 Diabetes
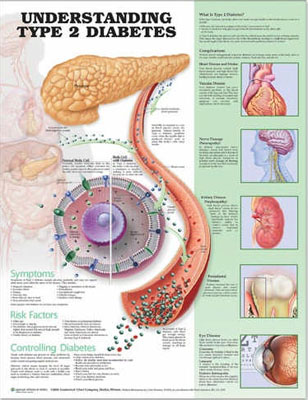
Diabetes is on the rise. The number of people diagnosed with diabetes every year increased from 1980 through to 2011 by 176%. Nearly all the new cases are Type 2 Diabetes, or adult-onset, the kind that moves in around middle age. Symptoms of Type 2 Diabetes include increased thirst, appetite, and need to urinate; feeling tired, edgy, or sick to the stomach; blurred vision; tingling or loss of feeling in the hands.
The causes of type 2 diabetes are complex and not completely understood, although research is uncovering new clues at a rapid pace.
However, it has already been proven that one of the reasons for the boom in type 2 diabetes is the widening of waistbands and the trend toward a more deskbound and inactive lifestyle in the United States and other developed countries. In America, the shift has been striking; in the 1990s alone, obesity increased by 61% and diagnosed diabetes by 49%.
For this reason, health experts encourage those who already have type 2 diabetes to start employing the wonders that exercise can do for them. Without exercise, people have the tendency to become obese. Once they are obese, they have bigger chances of accumulating type 2 diabetes.
Today, the U.S. Department of Health and Human Services reports that over 80% of people with type 2 diabetes are clinically overweight. Therefore, it is high time that people, whether inflicted with type 2 diabetes or not, should start doing those jumping and stretching activities.
Getting Started
The first order of business with any exercise plan, especially if you are a “dyed-in-the-wool” sluggish, is to consult with your health care provider. If you have cardiac risk factors, the health care provider may want to perform a stress test to establish a safe level of exercise for you.
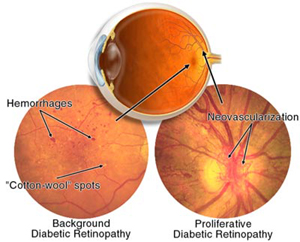
Certain diabetic complications will also dictate what type of exercise program you can take on. Activities like weightlifting, jogging, or high-impact aerobics can possibly pose a risk for people with diabetic retinopathy due to the risk for further blood vessel damage and possible retinal detachment.
If you are already active in sports or work out regularly, it will still benefit you to discuss your regular routine with your doctor. If you are taking insulin, you may need to take special precautions to prevent hypoglycaemia during your workout. Most people with insulin-treated diabetes notice that symptoms of hypoglycaemia change and become less obvious the longer they live with the condition, so extra precautions really are essential.
Start Slow
For those who have type 2 diabetes, your exercise routine can be as simple as a brisk nightly neighborhood walk. If you have not been very active before now, start slowly and work your way up. Walk the dog or get out in the yard and rake. Take the stairs instead of the elevator. Park in the back of the lot and walk. Every little bit does work, in fact, it really helps a lot.
As little as 15 to 30 minutes of daily, heart-pumping exercise can make a big difference in your blood glucose control and your risk of developing diabetic complications. One of the easiest and least expensive ways of getting moving is to start a walking program. All you need is a good pair of well-fitting, supportive shoes and a direction to head in.
Indeed, you do not have to waste too many expenses on costly “health club memberships,” or the most up-to-date health device to start pumping those fats out. What you need is the willingness and the determination to start exercising to a healthier, type 2 diabetes-free life.
The results would be the sweetest rewards from the effort that you have exerted.